An Integrated Approach Towards Better Patient Outcomes in Vietnam
In recent years, Vietnam has established itself as one of the most rapidly expanding economies in Southeast Asia (SEA) by displaying a robust history of economic advancements, investments in human capital, and infrastructure enhancements.
Within the healthcare industry, the market has made significant improvements which have resulted in better overall health conditions and life expectancy. The World Bank Group describes Vietnam as a “forerunner in the region”, having made huge progress towards accelerating Universal Health Coverage (UHC) through heavy investments from the Government.
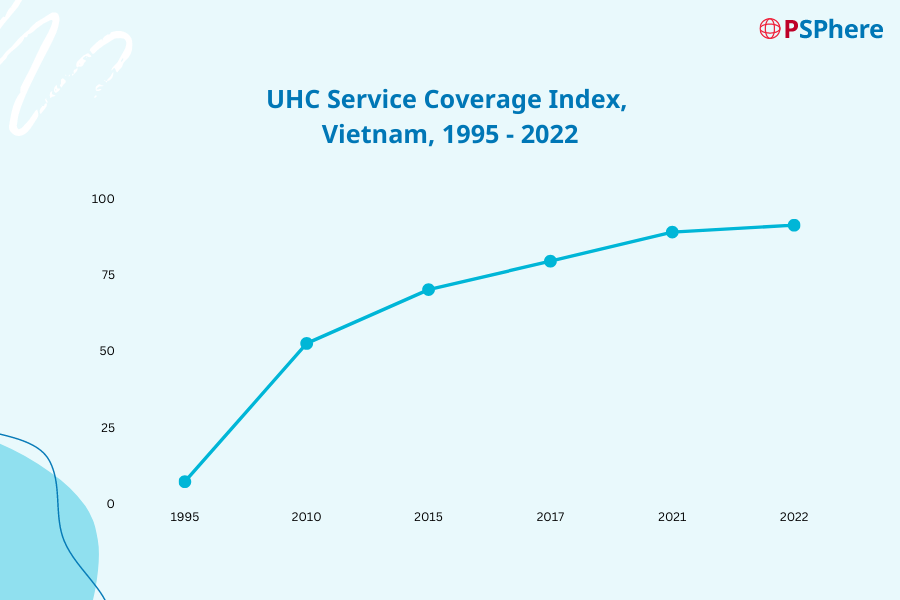
UHC is a concept that ensures every person, regardless of their financial or social status, has access to quality and affordable health services – including prevention, treatment, rehabilitation, and palliative care. Over the last 10 years (refer to Figure 1.1), the population covered under Vietnam’s UHC has increased significantly; from 52.4 million in 2012 to 91.1 million in 2022.
Navigating Population Growth and Changing Demographics
Vietnam has also made notable strides in population growth, ranking third across SEA and 15th globally, with a current population of 98.8 million which is projected to surpass 100 million by the end of 2024. As reported by the World Bank Group, its current life expectancy rate is at 75 years, with 7.7 percent of the total population being over 65 years old. Vietnam is on the cusp of an aging population, where the number of people over 65 is expected to rise to about 20.4 percent of the total population by 2050.
As the total population continues to grow, urbanize, and experience a shift in age distribution, we believe that there will be a surge in demand for health services, particularly for Noncommunicable Diseases (NCDs) such as cancers, cardiovascular diseases, diabetes, and chronic lung illnesses.
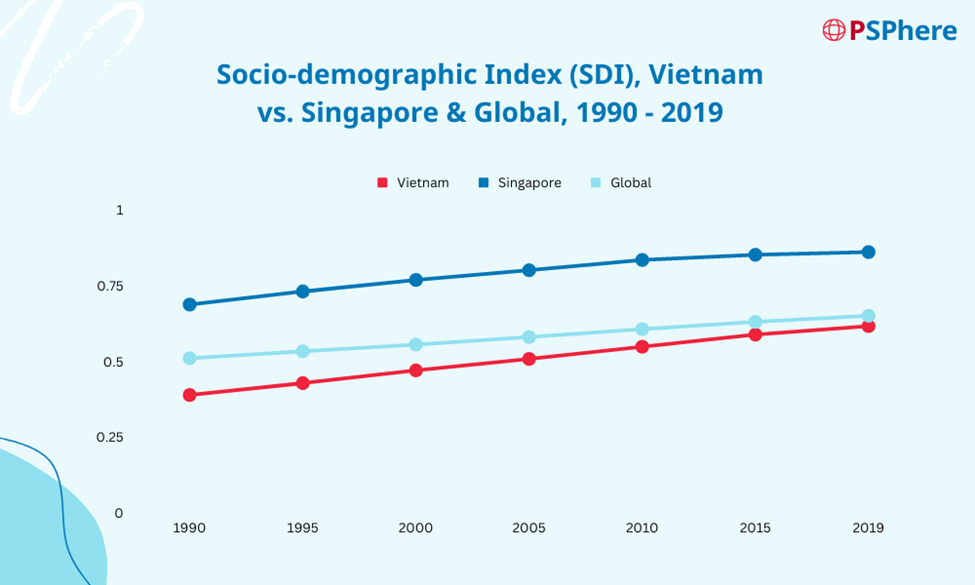
Figure 2.1 illustrates that Vietnam’s Socio-demographic Index (SDI) (in red) is slightly lower than the global average (in light blue), taking note that it has also been steadily increasing over the years. The SDI is a summary measure that identifies where markets or other geographic areas sit on the spectrum of development, considering income, education, and fertility rate, expressed on a scale between zero to one.
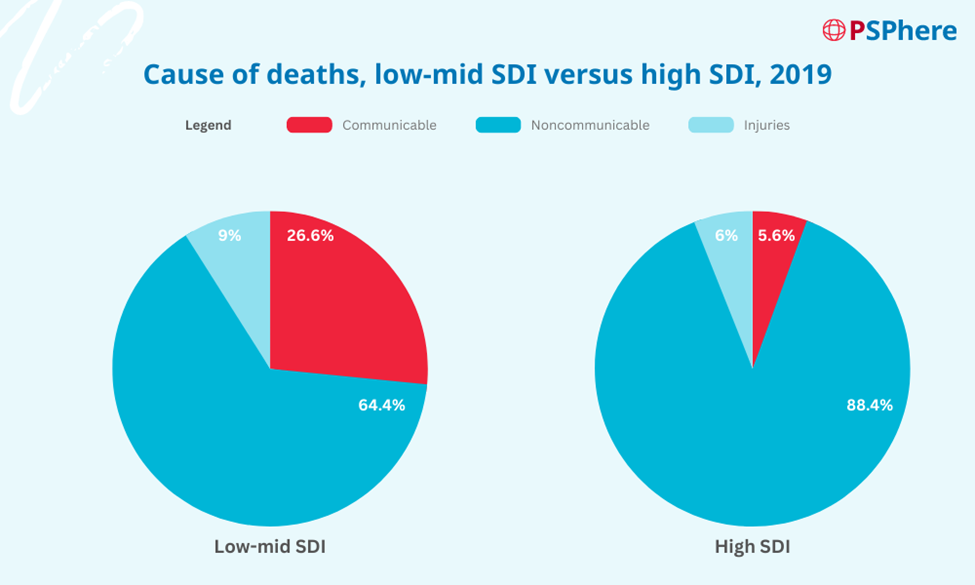
From Figure 2.2, we can see a clear distinction in the causes of deaths between a low-mid SDI market versus a high SDI market in which a larger percentage of deaths is associated with NCDs (about 24 percent more). As Vietnam inches towards being a mid-to-high SDI market, the healthcare industry must be prepared to handle the rise in such diseases and illnesses.
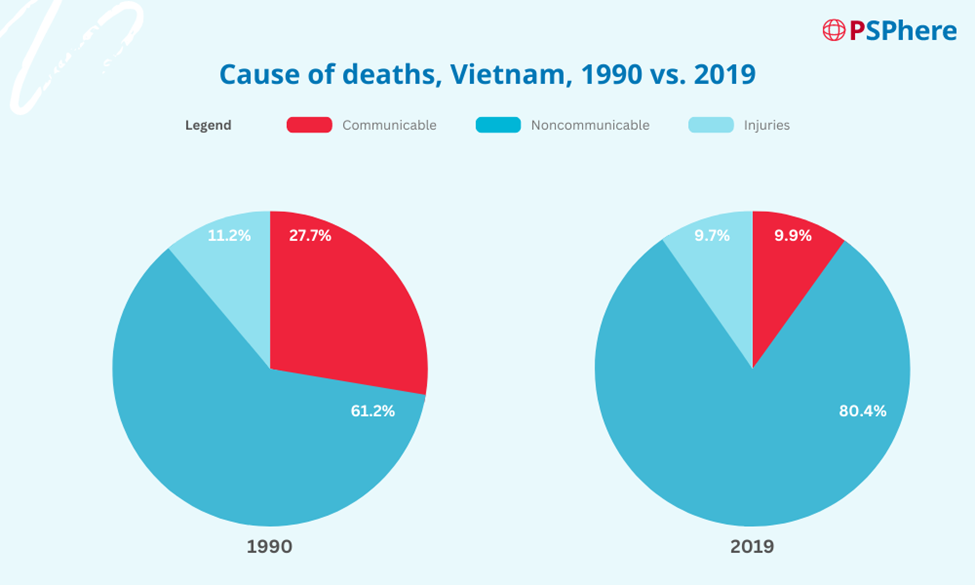
Looking at the evidence in Figure 2.3, together with the rising SDI in Vietnam (in Figure 2.1), we can already start predicting these trends. Patient support programs can play a crucial role in intervening and helping to lessen the burden on the national healthcare system. One method to handle this rise in demand for health services would be to implement programs to educate patients and empower them to take charge of their healthcare.
Improving Patient Adherence to Drive Better Treatment Outcomes
Patient adherence remains one of the key global problems across the healthcare industry, especially for chronic diseases in which patient adherence is estimated to only be about 50 percent in high-income markets, and much lower in low-mid-income markets.
According to G.D. Chauke et al (2022), poor adherence in low-mid-income markets is largely influenced by the lack of knowledge, negative attitudes, and negative beliefs. Today, patients can easily obtain information from various sources such as social media, friends, and relatives. However, as these sources are not verified, patients end up feeling confused and not adhering to their treatment plan. It is crucial tothink of strategies to change the public perception and improve patients’ lives.
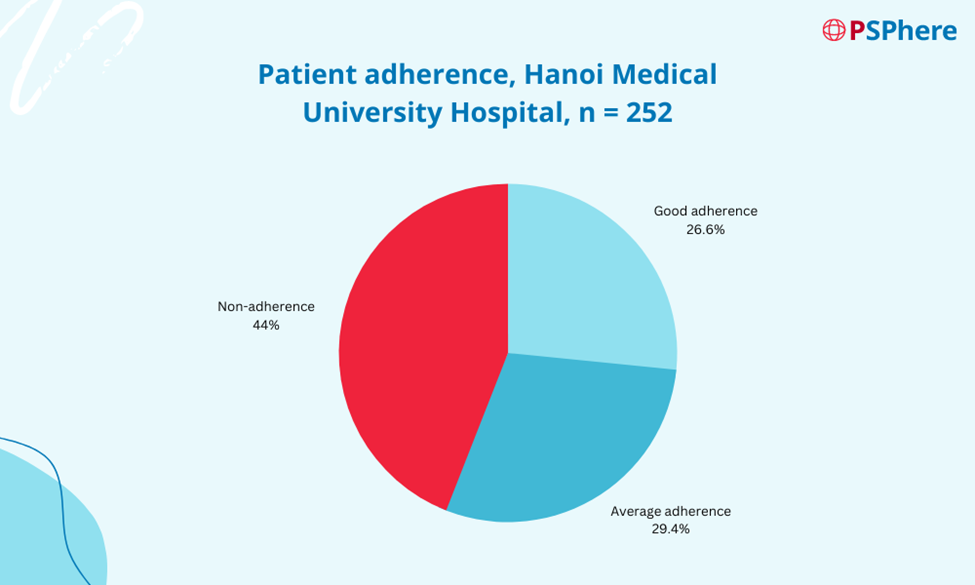
Earlier this year, a cross-sectional descriptive study assessing adherence to treatment plans was conducted at Hanoi Medical University Hospital examining 252 hypertensive patients. Hypertension is a leading risk factor associated with the burden of morbidity and mortality from cardiovascular diseases. Although 72.6 percent of these patients purchased the medication with their funds (with the remaining on insurance plans/others), only 55.95 percent of patients adhered to their treatment plan (refer to Figure 3.1).
Patients have also shared that oftentimes, they end up forgetting to take their medication; however, only 3.6 percent try to set a reminder for themselves. This study proves that patients are generally unaware of the severe complications that could arise with non-compliance with their treatment.
Encouraging Patient Adherence Through PSPhere
To address the issue of poor adherence and reduce the burden on the national healthcare system, we have carefully designed different components that can either be a standalone program or an add-on to other programs.
DKSH globally can offer the following adherence programs: (1) face-to-face visits, (2) video visits, and (3) educational portals. As we continue to work closely with our clients and patients, we will continue to develop better programs to improve patient outcomes.
In Australia, hospitals and respiratory clinics are grappling with severe capacity constraints, which have resulted in long waiting times for a specialist appointment of up to 17 months, even for some patients facing life-threatening situations. In addition, the COVID-19 pandemic has caused significant delays in many scheduled appointments–further exacerbating the situation and resulting in a large backlog of patients requiring care.
To address this pressing issue, in Australia, we converted an offline patient education program to a digitized program in 2021 alongside a key client of ours to ensure patients were still able to receive the care they needed without compromising on safety, particularly during the severe pandemic-related lockdowns. The program focuses on educating patients on managing their healthcare needs and providing them with tools and resources to take control of their health. Through empowering patients, we hoped to reduce further the strain on hospitals and clinics and improve access to care for those in need.
Our comprehensive program includes a range of services designed to provide optimal care and support to patients. This includes at-home nurse injection visits, medication deliveries, timely reminders, and convenient on-demand tele-support by our team of experienced and licensed nurse educators.

Our nurse educators play a vital role in our patient-centered approach by actively engaging with patients throughout their treatment journey. They diligently logged in each interaction and provided timely updates to the patient’s treating physician, including the recording, and reporting of adverse events. The program has been highly successful, with a global persistence rate of 95 percent and over 1,900 patients currently enrolled. To date, 62 percent of patients are fully equipped with the knowledge to conduct self-administration. This program was also recognized by the Australian pharmaceutical industry and won an award for Excellence in Patient Support and has since expanded to New Zealand where it continues to improve the lives of patients.
Long-Term Partnership to Bridge the Gap in Healthcare
The treatment of diseases often requires a multifaceted approach, that goes beyond receiving prescribed medication from doctors. At DKSH, we strongly believe that while medication is an important aspect of treatment, other aspects of care have a significant impact on patient outcomes. Stakeholders such as nurse educators, physical therapists, nutritionists, and psychologists, can play important roles in supporting patients and their families throughout their treatment journey.

DKSH Patient Solutions places patients at the center of their care journey, connect them to key stakeholders, and leverages technology to help them achieve better outcomes. In a patient-centric approach, which considers a comprehensive view of the patient’s health, key elements such as patient education, psychological assistance, nutritional counseling, and lifestyle adjustments are essential to a patient’s treatment plan.
In Vietnam, there are a multitude of methods one can use to communicate information to patients: television, radio, and print media. However, these methods are largely one-way communication methods and can entail difficulties in measuring the effectiveness of these programs. We are dedicated to addressing the challenges in the traditional healthcare value chain by providing technology to local partners we can bring together online (PSPhere) and offline capabilities (Patient Specialist Hub), to help improve patients’ experience and treatment outcomes by keeping them engaged through education materials and support. Reach out to us to learn more about our PSP solutions.
Sources:
- Việt Nam cơ bản hoàn thành mục tiêu bảo hiểm y tế toàn dân
- Universal health coverage (UHC)
- Health financing in Viet Nam
- UHC service coverage index – Viet Nam
- Vietnam Population 1950-2023
- Life expectancy at birth, total (years) – Viet Nam
- Aging in Vietnam: The elderly to account for 20.4% by 2050
- Global Burden of Disease Study 2019 (GBD 2019) Socio-Demographic Index (SDI) 1950–2019
- GBD Compare
- Factors influencing poor medication adherence amongst patients with chronic disease in low-and-middle-income countries: A systematic scoping review
- Đánh Giá Thực Trạng Tuân Thủ Điều Trị Và Một Số Yếu Tố Ảnh Hưởng Ở Người Bệnh Tăng Huyết Áp Khám Ngoại Trú Tại Bệnh Viện Đại Học Y Hà Nội
- Rural Australians are facing life-threatening wait times for medical specialists