Embracing a Hybrid Strategy: Integrating Online and Offline Capabilities to Enhance Patient Outcomes

“At DKSH Patient Solutions, we firmly believe in a hybrid strategy that combines digital interventions with in-person support to bring a holistic experience for our patients. We aim to not only resolve the immediate needs of our patients, but also help them achieve better outcomes in the longer-term.” said Ruch de Silva, Senior Director, DKSH Patient Solutions.
Over the years, we have witnessed a remarkable pace of technological evolution in both the realms of healthcare and patient care. Based on a report from Galen Growth, innovations have emerged across domains spanning from virtual health communities, medical diagnostics, healthcare logistics, digital health platforms (i.e., medical imaging), digital therapeutics, and on-demand lab tests. Collectively, these progressions have profoundly reshaped the healthcare landscape by increasing patient access, improving patient care, reducing healthcare cost, and streamlining inefficiencies.
While these technological leaps hold numerous merits, relying solely on them may fall short of providing comprehensive patient care. At DKSH Patient Solutions, we firmly believe in a hybrid strategy that combines digital interventions with in-person support to bring a holistic experience for our patients. We aim to not only resolve the immediate needs of our patients, but also help them achieve better outcomes in the longer-term.
In this article, Ruch de Silva, Senior Director, and Celestine Neo, Business Analyst, DKSH Patient Solutions, will delve into the potential of embracing a hybrid strategy for patient support, as opposed to favouring one approach over the other.
Patient Support Programs (PSPs) have come a long way, but there is need for further digitization
Patient Support Programs (PSPs), also known as Patient Assistance Programs or Patient Support Services, are initiatives designed to help patients better manage their medical conditions, navigate the healthcare system, and access the treatment and resources they need. In the early 1900s, PSPs’ initiatives primarily focused on providing financial aid, medical supplies, and basic healthcare services to underserved communities. These initiatives initially managed manually and were paper-based. As technology advanced, manually recording information on computers, became increasingly common.
Even today, these manual programs have not become completely obsolete as certain legacy programs are still being operated manually. However, these programs are not being executed with optimal efficiency in terms of man-hour and time spent, nor with the highest standards of compliance. Data stored on paper or in files does not guarantee privacy for patients and poses challenges for analysis and extracting meaningful insights from it. Another significant issue is the scalability of these programs.
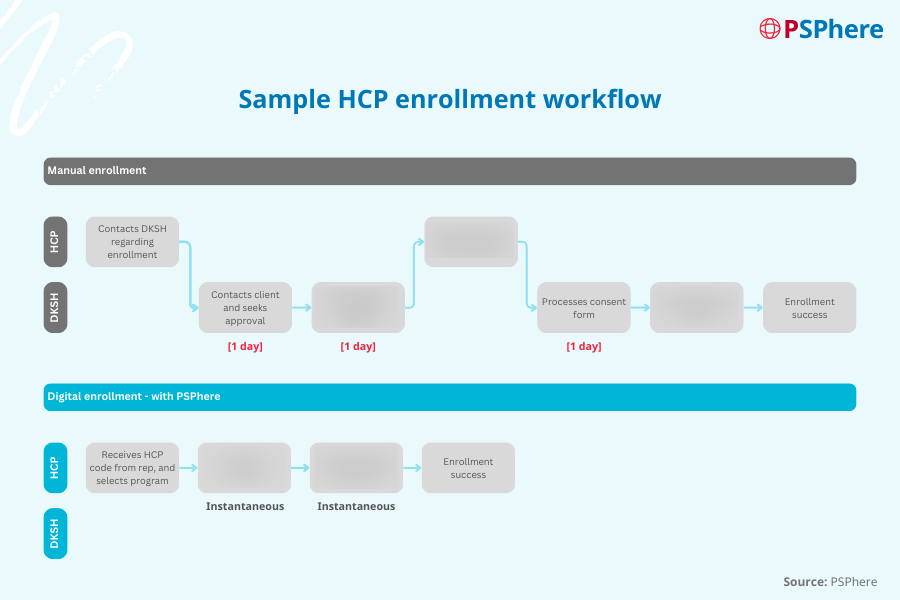
Fig. 1.0.: Sample HCP enrollment workflow – with and without PSPhere
Based on our experience, a process such as enrolling a Healthcare Professional (HCP) could previously take up to three business days due to the extensive paperwork needed. This prolonged process not only used resources inefficiently, but also can discourage potential users from PSPs altogether. With the introduction of technology, particularly the usage of our digital platform – PSPhere, we have managed to cut this process down to just one day (with reference to Fig. 1.0.). Given its increasing usage amongst stakeholders – patients, doctors, nurses, pharmacists, care-givers across Asia Pacific (APAC) markets ranging from Thailand to New Zealand, we have been continuously improving stakeholder engagement by solving real-world problems for them.
Market and investment enthusiasts have been shying away as we move past the pandemic
Relying solely on manual processes might not be the most efficient approach for PSPs. Likewise, exclusively pursuing a digital solution may not yield the best outcomes either.
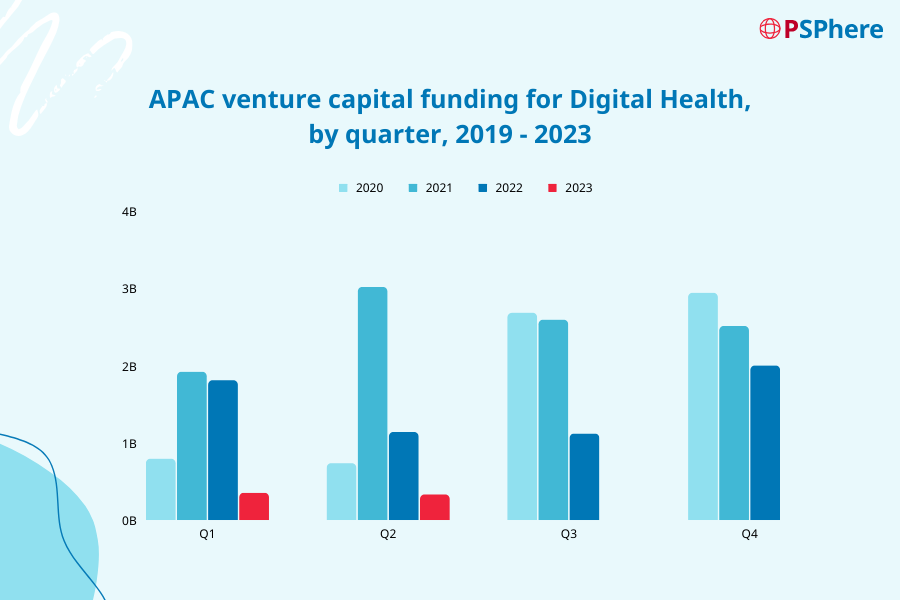
Fig. 2.0.: APAC venture capital funding for Digital Health, by quarter, 2019 – 2023 (Galen Growth, 2023)
As noted by Galen Growth, the first half of the year posed significant challenges for the Digital Health sector not only within the APAC region but on a global scale. With reference to Fig. 2.0., there is a strong correlation between the venture capital funding for Digital Health initiatives and the timeline of the COVID-19 pandemic. At the peak of the pandemic, there was a surge of investments in third quarter of 2020 as the world was going under lockdown and investors and suppliers of healthcare products and services needed to reimagine how healthcare was delivered. Digital Health led to great opportunities for HCPs to reach patients through other means, which paved the way for new approaches of patient care. At that time, venture capital and private equity firms were sitting on a record level of funds that have been raised by not yet deployed, which naturally led to the high investments at that juncture.
As we move beyond the pandemic, we are witnessing a shift in investment trends (with reference to Fig. 2.0.). According to Boston Consulting Group, there is a downturn in funding for Digital Health as investors are gradually shifting away from “exciting new ideas” to “demonstrated outcomes and evidence”. Initially, investors were willing to overlook the absence of profitability as long as revenue remained high; however, they are now seeking tangible returns.
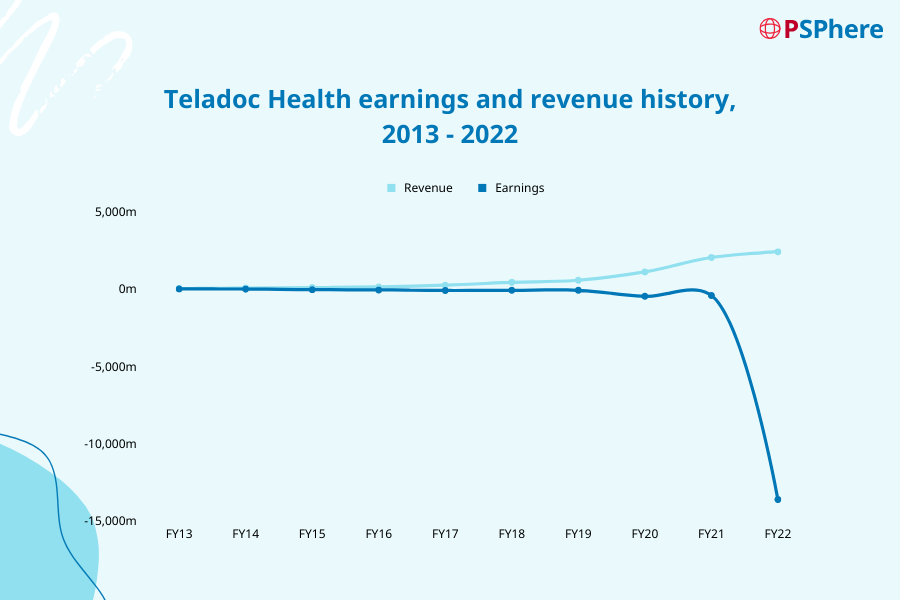
Fig. 3.0.: Teledoc Health earnings and revenue history, 2013 – 2022 (Simply Wall St, 2023)
An illuminating example is Teladoc Health, a prominent player in the Digital Health space, with a primary emphasis on telemedicine. Since their massive USD 18.5 billion acquisition of Livongo in 2020, the company has grappled with persistent profitability challenges. Fuelled by growing impatience, investors have taken the step of initiating legal action against Teladoc Health, alleging that the company provided misleading information to investors regarding its business, operations, and prospects.
Within the first half of this year, there was a heightened incidence of prominent bankruptcies, involving a few notable firms. Among them was Pear Therapeutics, a software-driven digital therapeutics platform. Pear Therapeutics focusing on tackling an array of conditions encompassing addiction, insomnia, post-traumatic stress disorder (PTSD), chronic pain, irritable bowel syndrome (IBS), and more. Its impact extended across the healthcare landscape, elevating the recognition of Digital Health with key stakeholders. Regrettably, a primary factor contributing to its eventual downfall rested upon the scepticism from numerous insurers, thereby disabling patients from receiving the care they required. Another key challenge lies within the operations. Certain patients have faced difficulties in downloading and using the application to receive their treatment. This proves that whilst technology may help to improve efficiency, it may not be the solution to everything.
We have seen successful plays in digital health, however, they have been piecemeal
Despite certain challenges, a strong interest persists within the realm of the Digital Health sector. This is supported by the discernible trend witnessed in the first half of 2023, which has marked a significant 1.2 times increase in partnerships compared to the same period in the previous year. This upswing in collaborative efforts reflect the industry’s unwavering drive to advance and innovate.
Ashkan Afkhami, Managing Director and Partner at Boston Consulting Group (BCG), provides valuable insights into the dynamics at play. According to Afkhami, “a pivotal transition in the sector’s trajectory hinges on the development of outcome-based solutions that can be substantiated through real-world evidence and comprehensive results”. This paradigm shift is crucial as it sets the stage for the eventual acceptance and integration of digital solutions by both payers and providers.
In the same report, Ami Karnik, Director and Venture General Manager at BCG, expounds a critical aspect of healthcare evolution. Karnik’s insights dive into the intricate balance between virtual and in-person care methodologies. She emphasizes on the significance of orchestrating a seamless fusion of these two care paradigms, an approach that holds the potential to yield multifaceted advantages for all stakeholders involved.
One notable integration of online and offline components is exemplified in the Continuous Glucose Monitoring (CGM) market. CGM has emerged as a pivotal tool for improving diabetes management, revolutionizing the approach compared to the conventional capillary blood glucose testing (CBG), or known commonly as self-blood glucose monitoring (SBGM). It provides real-time glucose trend information directly accessible on mobile platforms, eliminating the need for finger pricking.
Irace, et al., delve into the potential implementation of CGM in non-ICU hospital setting and assess the accuracy, effectiveness, and safety of CGM devices when compared to CBG. Their study concludes that when combined with offline patient monitoring components, CGM proves to be a dependable tool for enhancing glucose monitoring in non-critical cases.
Given that CGM data can be remotely accessed by patients, their HCPs, and designated caregivers, it enables continuous patient monitoring, facilitating an immediate feedback loop for patients and their HCPs; ultimately resulting in better treatment outcomes.
Our approach in combining online and offline across Asia Pacific to bring patients and healthcare stakeholders together
Much like the CGM example mentioned above, we believe that the effectiveness of a program rests upon the seamless integration of both online and offline approaches. By harnessing the capabilities of technology, we can enhance our patient engagement efforts and streamline operational workflows to attain heightened levels of efficiency. Conversely, the presence of in-person support is equally indispensable in ensuring the program’s overall success.
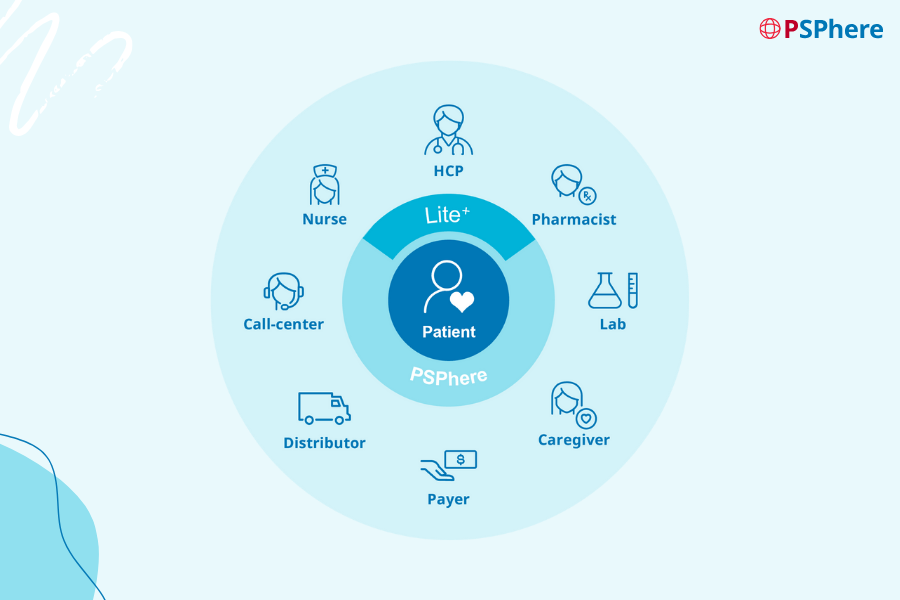
Fig. 4.0.: PSPhere wagon wheel
PSPhere, our digital platform, was developed with the intention of managing PSPs throughout the continuum of care for our patients. Anchored by our patient-centric approach, our primary objective is to establish patients as the focal point of care delivery. Through the seamless integration of key stakeholders – including but not limited to HCPs (such as doctors, nurses, pharmacists), caregivers, payers, delivery personnel, and our in-house Patient Support Specialists (PSS), we aim to revolutionize the landscape of treatment and care. Our conviction lies in the transformative potential of this approach, as it propels patient care into an all-encompassing ecosystem that seamlessly combines both online and offline capabilities.
Given DKSH Healthcare’s presence spanning across thirteen markets across Asia Pacific, encompassing locations such as Thailand, Vietnam, Taiwan, South Korea, Australia, and New Zealand, we can harness our expansive network of healthcare stakeholders within each of these regions. This positions us strongly to facilitate the connection between patients and their intended stakeholders.
Why we think blending online and offline will be game-changing for patients in Asia Pacific
We have placed strong emphasis on investing in both our digital platform and our people in each market, recognising their vital roles in the success of our programs.
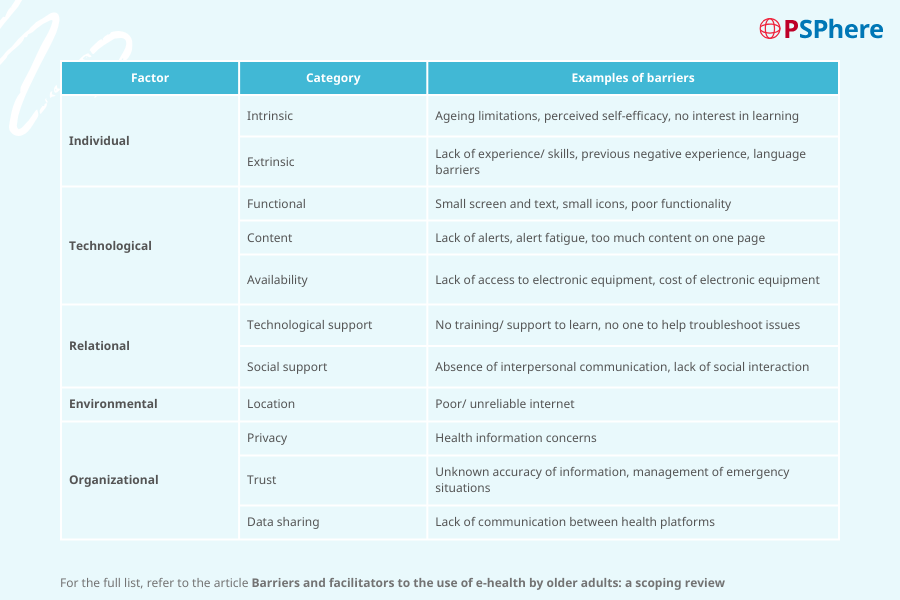
Fig. 5.0.: Example of barriers (Wilson, Heinsch, Betts, Booth, & Kay-Lambkin, 2021)
According to research on existing literature by Wilson, Heinsch, Betts, et al., “there are several barriers grouped into five categories associated to the adoption of Digital Health platforms for individuals aged 60 and above. Some of these barriers include the lack of experience and skills with Digital Health (or technology), previous negative experiences, or not having enough training and support” (refer to Fig. 5.0.).
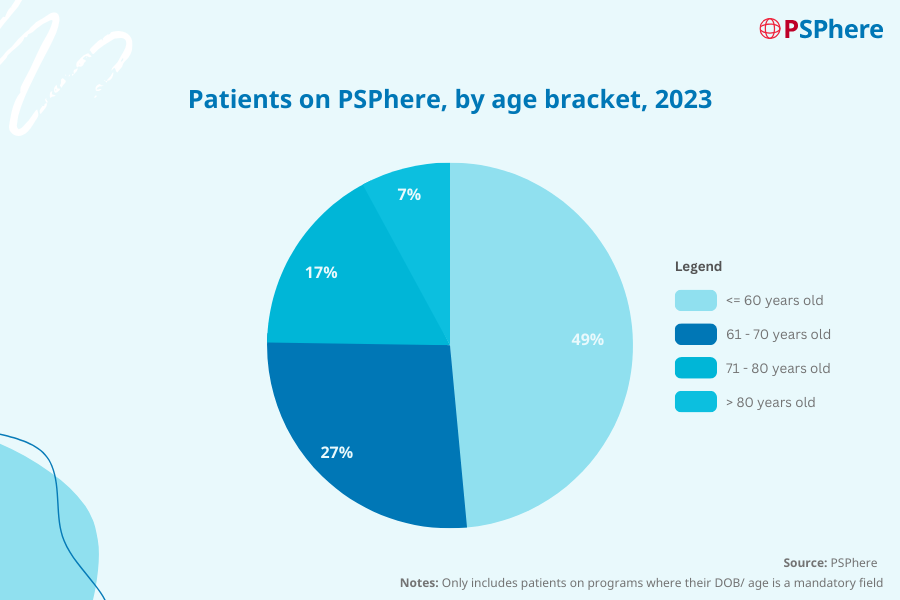
Fig. 6.0.: Number of patients on PSPhere – only programs where DOB/ age is mandatory
As about 51 percent of our patients are above 60, we believe that implementing our hybrid strategy will offer as an effective solution that can help these individuals overcome the majority of the barriers mentioned above. With most of our patients (above 60) being young seniors, we are confident that with some assistance from our local teams, they too would be able to successfully navigate our platform for their program needs.
To ensure that all our patients receive timely assistance, PSPhere offers a seamless connection to our dedicated team of Patient Support Specialists – all of whom are qualified nurses proficient in the patient’s native language. This personalized approach is particularly significant, as providing patients with a dedicated voice of concern has been proven to be reassuring, especially in times of need. Our patients can take comfort in knowing that we are actively alongside them on their journey towards better health.
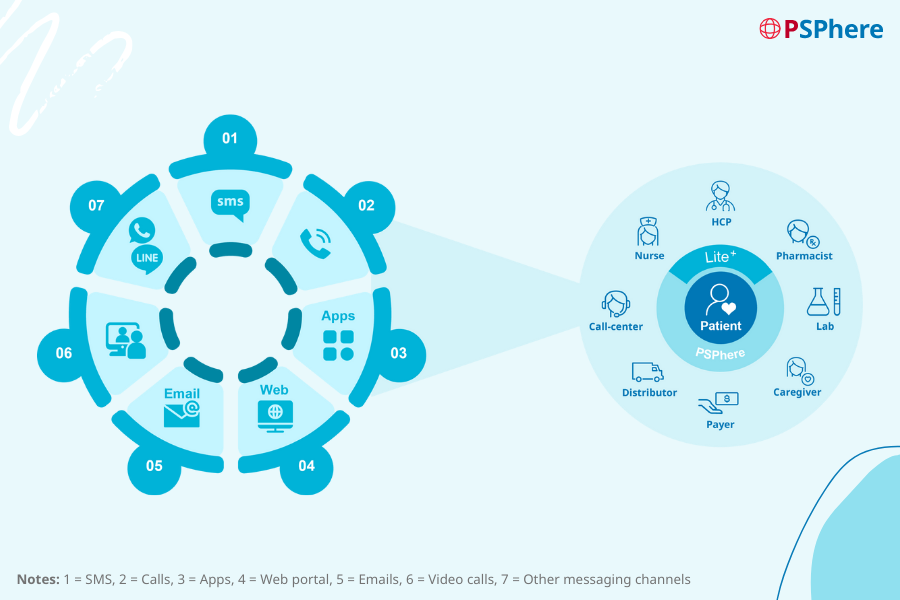
Fig. 7.0.: Omni-channel patient engagement through PSPhere
Leveraging the robust and secure integrations available within PSPhere, we have the capabilities to engage with our patients through their preferred communication channel of choice. This minimizes the need for patients to adapt to a new program or technology, allowing them to remain comfortable with what they are already accustomed to. For example, our patients in Thailand may continue using LINE to communicate with our Patient Support Specialists, eliminating the need to download an entirely different messaging platform. Depending on individual preferences, patients may also opt for calls or emails instead.
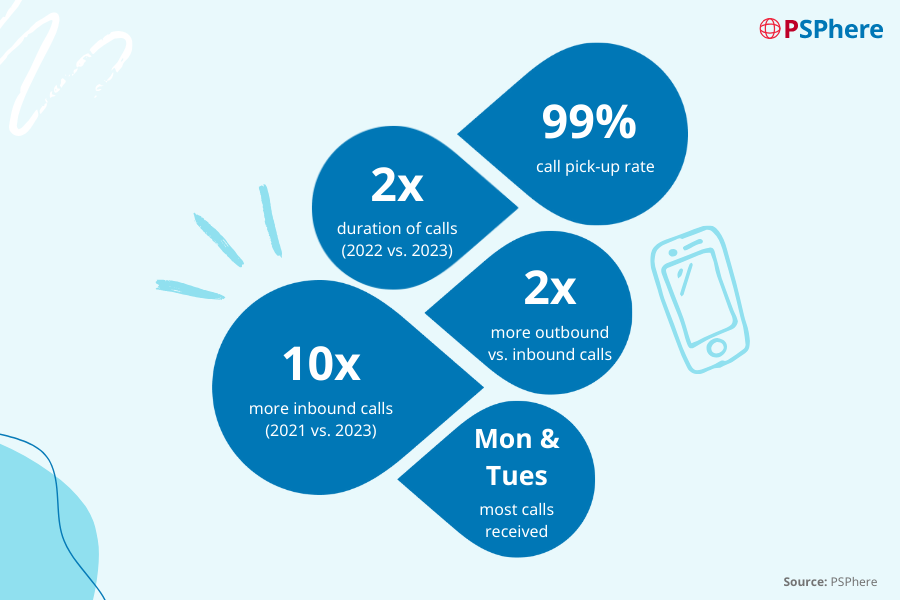
Fig. 8.0.: Patient engagement statistics from PSPhere
Based on our experience, we have observed a consistent upward trend in both call volume and duration over the years. This trend serves as a clear indicator of the success of our programs, which have witnessed steady growth in terms of both the programs we offer and the number of patients under our care.
The outbound calls our Patient Support Specialists mainly consists of welcome and follow-up calls. Notably, we make twice as many outbound calls as inbound ones, demonstrating our commitment to proactively engage with our patients throughout their healthcare journey.
Our commitment to excellence extends beyond the efficient operation of our programs. As highlighted in the study conducted by Wilson, Heinsch, Betts, et al., one of the significant barriers identified pertains to data sharing and privacy concerns. At DKSH Patient Solutions, we prioritize the security of patient data on our platform.
To ensure this, our team undergoes rigorous training, equipping them with the necessary skills to handle adverse events and promptly address incidents relating to both the platform and the program. We are committed to stringent compliance standards, ensuring that all actions taken are not only efficient but also fully compliant with data privacy regulations – keeping both you and our patients safe. We will explore this in further detail in upcoming articles.
Building trust, starting with our clients – pharmaceuticals and medical device manufacturers
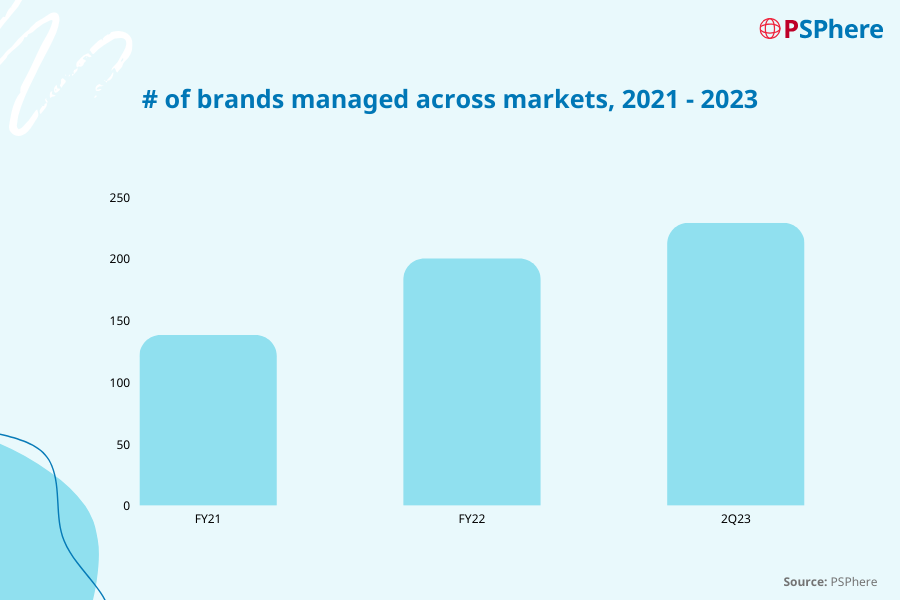
Fig. 9.0.: Number of brands managed, 2021 – 2023
Along the years, we have launched at least one program with 14 out of the top 21 leading pharmaceutical multinational corporations. Our achievements go beyond expanding our client base; we are also expanding on the number of brands managed by our teams. On average, we oversee six brands per pharmaceutical company in a country, which illustrates the trust and confidence our clients place in us to effectively manage their PSPs.
In conclusion, combining both the strengths of online and offline approaches stands as a testament to our commitment in delivering effective and compliant PSPs. Our journey towards achieving excellence is far from over, and we remain steadfast in our pursuit of innovative solutions that not only meet but exceed the expectations of our partners and patients.
References
- Boston Consulting Group. (2023). The Future of Digital Health.
- Cherry, S. (1997). Before the National Health Service: financing the voluntary hospitals, 1900-1939. Economic History Review, 305-326.
- Datalla Group. (2023). Pear Therapeutics: A Wake-Up Call for the Digital Health Industry? Retrieved from LinkedIn
- Galen Growth, (2021). Pharmaceutical Digital Health Innovation Index, Global Digital Health 2021.
- Galen Growth. (2023). Digital Health Funding H1 2023 – Global Must-Know Trends & Insights.
- Galen Growth. (2023). Global Digital Health Innovation Ecosystem Report H1 2023 Key Trends.
- Irace, C., Coluzzi, S., Cianni, G. D., Forte, E., Landi, F., Rizzo, M. R., . . . Consoli, A. (2023). Continuous glocose monitoring (CGM) in a non-Icu hospital setting: The patient’s journey. Nutrition, Metabolism & Cardiovascular Diseases.
- Jennings, K. (2023). Pear Therapeutics Files For Bankruptcy As CEO Blames Shortfalls On Insurers. Retrieved from Forbes
- Ladika, S. (2023). What Does Pear Therapeutics’ Bankruptcy Mean for PDTs? Retrieved from Managed Healthcare Executive
- Landi, H. (April, 2020). Digital health investments were off to a record start. How will COVID-19 change things? Retrieved from Fierce Healthcare
- Landi, H. (October, 2020). Teladoc finalizes blockbuster deal with Livongo in less than 3 months. Retrieved from Fierce Healthcare
- Landi, H. (June, 2022). Teladoc hit with lawsuit alleging it misled investors after ‘significant losses’. Retrieved from Fierce Healthcare
- Landi, H. (July, 2022). Teladoc takes hefty impairment charge in Q2 with losses mounting to nearly $10B. Retrieved from Fierce Healthcare
- Park, A. (2023). Pear pulped: Digital therapeutics maker’s assets sold for $6M at auction after bankruptcy filing. Retrieved from Fierce Biotech
- Simply Wall St. (2023). NYSE: TDOC Stock Report. Retrieved from Simply Wall St
- Teladoc Health. (2023). Teladoc Health’s Investor Relations. Retrieved from Teladoc Health
- Usoh, C. O., Kilen, K., Keyes, C., Johnson, C. P., & Aloi, J. A. (2022). Telehealth Technologies and Their Benefits to People with Diabetes. Diabetes Spectr. doi:10.2337/dsi21-0017 Wilson, J., Heinsch, M., Betts, D., Booth, D., & Kay-Lambkin, F. (2021). Barriers and facilitators to the use of e-health by older adults: a scoping review. BMC Public Health